In the wake of recent vaccination efforts, the Spanish Government had some hopeful projections: Assuming there will be no unforeseen events, the target of vaccinating 70% of the adult population during the summer would appear to be possible – at least in terms of the number of available doses.[1]
To date, nearly 1 and a half billion doses (1,451,876,531 doses 17th of May 2021) of coronavirus vaccines have been administered around the world.[2] The graphics below[3] show the daily vaccine doses administered per 100 people (in orange) and the share of people who have received at least one dose of a COVID-19 vaccine (in blue).
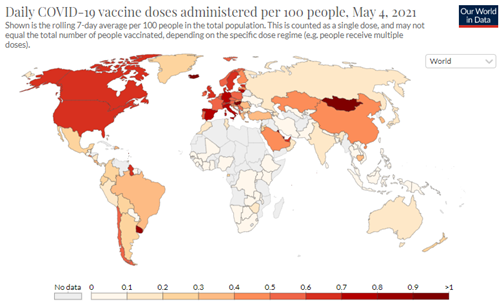
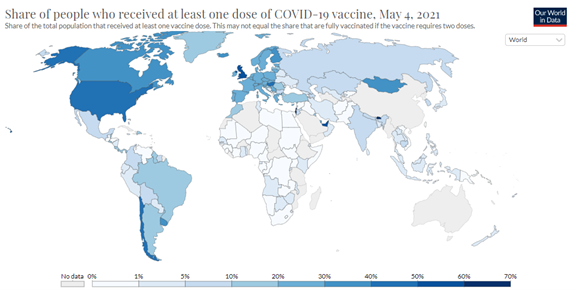
Stand out countries, as you may know, are the United States and the United Kingdom, with a vaccination rate of 44% and 51%, respectively, as well as Chile with 42%, the United Arab Emirates, also with 51%, and Israel and Bhutan, both at 62%
But even with so much attention paid to the why, how, and when of vaccines, you might still easily find yourself confused on the different types of vaccines, how they work, and what exactly distinguishes them from one another. Not all inoculations are created equal.
We have put together a brief overview of the vaccinations currently available or under development in different parts of the world.
At the moment there are 5 different types of vaccines used to provide immunity against COVID-19:
- Genetic Vaccines:
Vaccines that deliver one or more of the coronavirus’s own genes into our cells to make them produce viral proteins, which then provoke an immune response.
- mRNA vaccine: Pfizer (US) / BioNTech (Germany); Moderna (US); CureVac (Germany)
- DNA vaccine: Zydus (India)
- Viral Vector Vaccines:
Vaccines that contain viruses engineered to carry coronavirus genes. These modified harmless viruses enter cells and make them produce coronavirus proteins, which then provoke an immune response.
- Adenovirus: Sputnik V (Ad5+Ad26, Russia); Oxford AstraZeneca (ChAdOx1, British-Swedish); CanSinoBIO (Ad5, China); Johnson&Johnson (Ad26, US)
- Protein-Based Vaccines:
Vaccines that contain coronavirus proteins but no genetic material. Some vaccines contain whole proteins, and some contain fragments of them. Some pack many of these molecules on nanoparticles.
- Bektop (Russia); ZFSW (China); Novavax (US); IFV (Cuba); MedicagoGSK (Canada); Abdala (Cuba)
- Inactivated or Attenuated Coronavirus Vaccines:
Vaccines created from weakened coronaviruses or coronaviruses that have been killed with chemicals.
- BBIBP (China); Sinovac (China); WIBP (China); BharatCovaxin (India); IMD (China); RIBSP (Kazakhstan)
- Repurposed Vaccines:
Vaccines already in use for other diseases that may also protect against Covid-19.
- BCG (tuberculosis vaccine)
To understand how any of these vaccines work to induce protective immunity against SARS-CoV-2 within us and prevent COVID-19 disease, a basic view of how a virus infects organisms and how our immune system respond to this, is necessary.
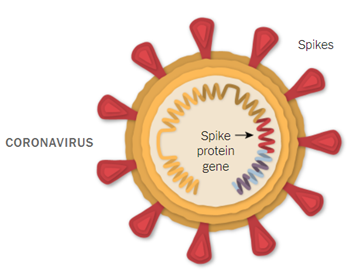
Put simply, when a virus enters our body, it invades cells to survive and replicate. Virally infected cells produce viral proteins and induce an extensive array of defence mechanisms including (1) immune cells that can recognise virally infected cells and kill them, and (2) neutralising antibodies that bind free viral particles specifically by recognising viral structures (i.e., the Spike protein), and therefore block infection.
Importantly, even once the infection has been cleared, memory immune cells specific to the particular pathogen remain in the body. This means that if we are exposed to the same virus again, the tailored immune response can happen much faster, resulting in a shorter and less severe disease course. This is the essential mechanism, which we have learned to take advantage of in order to artificially induce immunity to other viruses including measles, hepatitis B, and smallpox.
Knowing this, the following sections illustrate in more detail how each of the vaccine-types function in the body. They all work by exposing healthy people to the inactivated virus or parts of it (i.e., the Spike protein), by imitating the infection they allow the immune system to develop cells and antibodies specific to the harmful virus. In this way, the body is trained to fight the virus and responds swiftly and efficiently when exposed to the real disease.
Genetic/ mRNA Vaccines
(Pfizer/BioNTech, Moderna)
These vaccines use innovative technology that reached commercial-stage for the first time with the COVID-19 vaccines. In the case of Pfizer’s and Moderna’s vaccines, an mRNA encoding for the Spike protein is wrapped inside lipid nanoparticles that will be taken up by the body’s front-line immune cells. Once taken up, the cell can read the genetic material from within the nanoparticles to produce the Spike protein. The Spike protein is presented on the cell’s surface to be recognised by immune cells, which triggers a specific immune response as if the body were going through an actual viral infection. The desired effect is achieved, since memory immune cells and long-lived antibodies are produced, which help rapidly fight the virus in the future before it can spread and cause illness.
It is important to note that the viral genetic material does not incorporate in the body’s own genetic material, and the vaccine’s components degrade relatively fast within the body.
Viral Vector Vaccines
(AstraZeneca, Sputnik, Johnson & Johnson)
This type of vaccine uses viruses that are harmless to humans as vessels to enter the body and make host cells to produce a piece of the disease-causing virus. Some vaccines recently used for Ebola outbreaks have used viral vector technology, and advanced clinical trials are underway for other diseases, including HIV and Zika.
For Covid-19 vaccines, a piece of DNA encoding for the Spike protein is added to the genome of an adenovirus, which are common viruses that typically cause colds or flu-like symptoms. Vaccines use a modified version of adenoviruses that can enter cells but cannot replicate inside them. Once the virus has entered the cell, it breaks down and the genetic information within it that encodes for the Coronavirus’ Spike protein is released. It can then be transcribed by the body’s cells Spike proteins are produced and subsequently presented on the cell surface, to be recognized by the immune system.
The principle is similar to that of mRNA vaccines, however, the genetic material and the way through which it enters the human body differs. Once again, neither the harmless virus nor the genetic material it carries are incorporated into the body’s own genetic information, and they are eventually eliminated.
Protein-Based Vaccines
(Novavax)
Although slower to develop, protein-based vaccines are well understood with a strong record of safety and effectiveness (e.g., hepatitis B, HPV (human papillomavirus) and meningococcal B vaccines).
This vaccine type does not carry any genetic material but contains proteins unique to the virus. For Covid-19 vaccines, the Spike protein is produced in vitro in lab conditions and is then assembled in nanoparticles together with an immune system-activating adjuvant. These nanoparticles are what is injected into the body in the vaccine, and work by inducing a robust immune response against the Spike protein they carry. Since it is only the Spike protein and not the entire virus that enters the body, these vaccines are incapable of causing disease and no infection occurs.
Inactivated Virus Vaccines
(Sinopharm, Sinovac, Bharat)
This vaccine type may be the oldest way of vaccination that exists (e.g., hepatitis A, flu, polio, rabies). Large stocks of the coronavirus are grown and inactivated (or killed) so they can no longer produce the disease. Their proteins, however, including the Spike protein, remain and can still be recognized by the immune system. Thus, while there is actual coronavirus entering the body, it cannot produce a harmful infection, since it has been inactivated. Nevertheless, immune cells can spot it and develop immunity to it, in preparation for a ‘real’ infection with live coronavirus.
Coronavirus Variants and Mutations
Each coronavirus contains nearly 30,000 letters of RNA that encode for ~30 proteins. When the virus infects cells, it hijacks them to make millions of copies of itself. As an infected cell makes new coronaviruses, it occasionally makes tiny copying errors called mutations. These random single-letter alterations that occur when making copies of the viral RNA can be neutral, beneficial or detrimental to the virus. Mutations of concern are those that alter viral proteins in a way that improve the virus’s ability to spread or cause disease.
Covid-19 is caused by a coronavirus strain known as SARS-CoV-2. Over the course of the pandemic, a number of variants of SARS-CoV-2 have arisen (i.e., UK, South Africa or Brazil variants). A variant is a group of SARS-CoV-2 viruses that share the same inherited set of distinctive mutations. Some of the potentially problematic consequences of emerging variants are, (1) ability to spread more quickly in people, (2) ability to cause either milder or more severe disease in people, (3) ability to evade detection by specific viral diagnostic tests, (4) decreased susceptibility to therapeutic agents, and (5) ability to evade natural or vaccine-induced immunity.
Therefore, the development of new variants and the vaccines’ effectiveness against them (as well as treatment and containment measures) are something to monitor closely.
[1] Heather Galloway, El País, 02/04/21 https://english.elpais.com/society/2021-03-02/will-spain-be-able-to-vaccinate-70-of-the-adult-population-by-the-end-of-summer.html
[2] Covid-19 vaccine tracker: The global race to vaccinate. (n.d.). Financial Times. Retrieved 17 May 2021, from https://ig.ft.com/coronavirus-vaccine-tracker/
[3] Coronavirus (COVID-19) Vaccinations—Statistics and Research. (n.d.). Our World in Data. Retrieved 5 May 2021, from https://ourworldindata.org/covid-vaccinations
